Hello, my name is Rhabdo, short for Rhabdomyolysis. Now, before anybody jumps off the bridge, you might want to grab a parachute in order to potentially ease the fall. I know I am strongly associated with current fitness trends and protocols, but I want to provide everyone with real knowledge. The information presented here is not an intentional jab at any given person or groups of individuals, but merely serves as an educational and informative piece of my history. Since I don’t have a last name, please just can call me Rhabdo.
In the fitness and strength communities, most everyone depicts me as an exhausted semi-cartoonish (yet well-muscled) clown, who is always connected to a dialysis machine. I’m always standing next to some workout equipment with my bowels falling out on the floor and with blood everywhere as if it were a Valentine’s Day massacre. Sometimes, however, I even hold a puke bucket. My literal meaning is the breakdown of muscle tissue (9). Although a broad definition, I am more commonly used to describe characteristics of skeletal muscle degeneration due to injury, traumatic or non-traumatic origins leading to muscle breakdown and cell death. According to some science, my history dates back thousands of years (17). In fact, in the early part of the 20th century, some cases were even documented after the Sicilian earthquake in 1908 and in the German military literature after World War I (6). Even British physicians reported cases in bombing victims in 1940.
What causes me and how do I work?
Now, there are slight differences in terms. There is me, Rhabdomyolysis, and my other brother, Exercise-induced Rhabdomyolysis. While the physiological impact of what happens in the muscles are nearly identical, my initial causes are not always similar. Major causes include crush injuries, burns, infections, medications, drugs, and intense exercise. Misdiagnosed or left untreated, I can result in severe complications such as acute renal failure (ARF), hypocalcemia, hyperkalemia, hypervolemia, muscle necrosis (death), cardiac abnormalities, and compartment syndrome (14). Yes, it’s nasty stuff. On the other hand, my brother, Exercise-induced, sometimes referred to as Exertional Rhabdomyolysis (ER) occurs in response to excessive, prolonged, or extreme repetitive exercise (12). The exercise-induced portion is one of my most common forms. I’m regularly observed after extreme, intense exercise, and even from incorporating eccentric muscular contractions, due to increased strain placed on the muscle tissue causing muscle damage to the muscle fiber (16). However, I want to clarify that emphasizing some eccentric contractions into your training to promote strength and size is NOT going to unleash my beast.
It all starts in the sarcolemma and initiates a rise in intracellular calcium, caused directly by muscle injury or disturbance in energy expenditure. Excess calcium concentration results in a destructive interaction between the contractile proteins, actin and myosin, leading to fiber necrosis (fiber death; yes that’s a bad day for you), and cell death. Muscle proteins, including creatine kinase (CK) and myoglobin (MB), are released into circulation. Science has briefly described the role of increased myoglobin levels in the blood that dumps into the urine (16). Consequently, the occurrence of myoglobinuria (dark urine) travels directly to the kidneys, causing individual renal failure, which is rarely seen (I’m only very mean when you piss me off). Myoglobin, the oxygen-binding protein in muscle, is increased with skeletal muscle injury and excreted through the kidneys. Myoglobin released from damaged tissue can precipitate in the kidney, block renal tubules and ultimately may contribute to complete kidney shut down (15). The myoglobin released by the damaged muscle will discolor the urine to a reddish brown color. Perhaps the most common ailments are changes in cellular metabolism. With increasing work and muscle exhaustion, it increases sarcoplasmic influx of sodium, chloride and water occurs, resulting in swelling. Calcium also enters into the cell in exchange for intracellular sodium. Calcium stimulates phospholipase A2, leading to production of reactive oxygen species (AKA, free radicals that damage shit). Such a cascade of events leads to severe inflammation, pain, and swelling.
I can be life threatening due to not only renal failure, but also due to hyperkalemia (massive potassium elevation) and disseminated intravascular coagulation (lots of small blood clots which you don’t want). Other factors such as alcohol abuse, drug overdose, prolonged immobility or unconsciousness are also indicators of my disease.
Although my condition is rarely localized, it has been reported (9) that consistent exercise risk factors for developing me appear to be those who have low baseline fitness (i.e. untrained) levels and premature use of highly repetitive exercises (e.g. squats, push-ups, sit-ups), and/or throughout exercise in extremely hot or humid conditions, and is quite common in military personnel. A common cause in those that catch me seems to be exertion past the point when fatigue and utter exhaustion would require the person to naturally stop. One small example reported (9) extreme exercise leading to my outrage where persons were exposed to doing hundreds of push-ups in an afternoon or “squat jump syndrome”, where individuals were told to squat as low as possible and then jump as explosively as possible repeatedly until complete exhaustion. One point I must make is that although I’m highly linked to extreme exercise protocols and regimens, I can actually occur from relatively 'safe' exercise too (I know, it sucks!) because some people are just more prone to me.
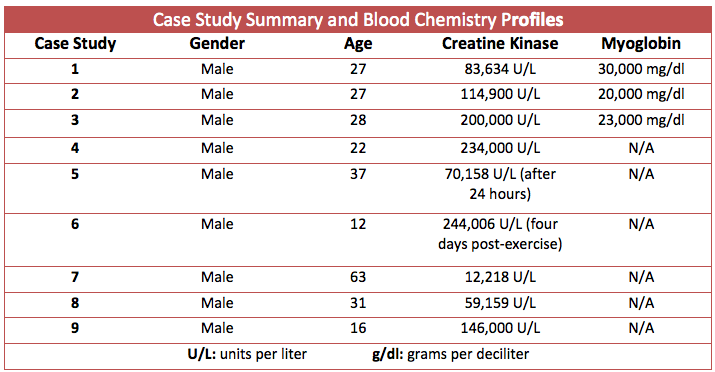
It’s important to distinguish between delayed onset muscle soreness (DOMS), and exertional rhabdomylysis. After regular and normal bouts of resistance training, delayed onset muscle soreness (DOMS) occurs. The intensity of DOMS increases within the first 24 hours post-exercise, peaks between 24 and 72 hours, and eventually disappears within days (2, 4). One of the hallmarks of DOMS and an indirect marker of muscle damage is increased serum creatine kinase (CK) levels. Normal serum CK levels are usually 20 to 200 U/L (units per liter); (5000 U/L is indicative of serious disturbance to the muscle (1) and greater than 10, 000 U/L is indicative of me (14-16). Even unaccustomed high-intensity resistance training can cause an individual’s serum CK level to abnormally increase well above 5000 U/L. However, what’s interesting and not as common knowledge as many think is that science has classified individuals as ‘‘high responders,’’ ‘‘low responders,’’ or ‘‘no responders’’ based on their creatine kinase activity after exercise (1, 2, 4). However, I want to point out that just because your creatine kinase levels are elevated doesn’t automatically mean you caught me. There are signs and symptoms.
Signs and Symptoms
Whenever somebody catches me, I initiate some classic symptoms, which include reddish-brown (cola-colored) urine, muscular pain and weakness. Reddish-brown urine may indicate myoglobinuria (presence of myoglobin in the urine) and can be a powerful diagnostic tool for somebody that knows that caught me (6). Reddish-brown urine, however, is present in only about half the cases of my presence, although its absence does not rule me out (6). Unfortunately, muscular pain and weakness are nonspecific, subjective and commonly experienced after intense and/or unaccustomed exercise without adverse effects. Other symptoms include muscle stiffness and swelling (6).
Who can catch me?
As previously mentioned, factors for developing me are mainly those with low baseline fitness (i.e., untrained) levels and premature use of highly repetitive exercises and/or throughout exercise in extremely hot or humid conditions, and those in the military. Some reports have indicated that my acute condition can strike about one out of every 300 military recruits during their first week of training.
However, some genetic differences may predispose certain individuals and thus are more prone in catching me. Many of these genetic differences result in the deficiency of enzymes important in ATP production or calcium handling. For example, McArdle disease can increase susceptibility of catching me because of reduced ability to utilize glycogen to make ATP (9). Another example is Carnitine polmitoyl transferase II (CPT2) deficiency: CPT2 is an enzyme required for long-chain fatty acids to enter the mitochondria (for ATP synthesis) where they may be broken down for energy. Those that have this genetic deficiency appear to have an increased risk of catching me because of reduced ability to produce ATP from fat (9). Moderate cases of me are also are common after triathlons.
Here’s the thing, I know that whenever I come up in the media or various social media outlets, it always concerns CrossFit. Every time something happens and my name comes up, it’s more or less linked with CrossFit. While this is true, however, to be honest and fair, I’m NOT just a CrossFit disease. Even highly trained people can get me. In many cases, folks with a strong fitness base who have an ability to perform but don’t necessarily have the recent training volume to support gregarious volumes of work can get me. Surprisingly, those who experience me can and are very fit, although it’s less common. One of the many caveats of my disease is that scientific researchers are just unable to perform experimental research to produce my condition. This is why case reporting is the sole factor in knowing about my condition.
Case Reports
There have been numerous case studies describing multiple incidents of my disease (7, 8, 11, 16). These studies share commonalities such as hospitalization, elevated creatine kinase levels, elevated myoglobin content, dark-colored urine, excessive pain and swelling. A recent case report was published of a male athlete/exercise physiology professor who started a high-intensity resistance training program after a period of detraining (13). The high-intensity resistance training exercise session, which elicited my condition, included 48 alternating sets (60 seconds duration) of push-up and pull-up variations.
This person who caught me performed the maximum number of repetitions possible of push-ups or pull-ups in each set. The total exercise duration was 48 minutes. He performed approximately 400 push-ups and approximately 200 pull-ups in 48 minutes. Within one hour after the exercise session, I started to take over his body, as he had difficulty moving his arms and upper body. Although he was experiencing intense pain the next day, he went to work and played ice hockey at night. If that wasn’t enough, the following day, he performed a lower body high-intensity workout. He urinated halfway through this session and described “cola-colored” urine (see how I work now!). When he was diagnosed, the attending physician revealed positive urine myoglobin and elevated blood creatine kinase (CK) levels of 59,159 U/L. On the fourth and fifth days of hospitalization, he received acupuncture treatments. Three weeks later, his CK level was still elevated (approximately 5000 U/L). One month after the diagnosis, he slowly returned to high-intensity resistance training (two times per week) without any complications.
In the case of a healthy adolescent athlete (67.9 kg, height = 165.5 cm), he participated in a three day preseason wrestling camp, which resulted in hospitalization and diagnosis of my condition. As part of the pre-season “conditioning” program directed and supervised by his “coach”, the 16 year-old completed 60 minutes of short, intense intervals of wall-sits, squats, sit-ups, push-ups, lunges, and plyometric jumps. On the following day the athlete continued his vigorous training consisting of running drills. Unfortunately, that night is when it all started (do you see my pattern?) as he noticed dark brown urine, the color of cola. The day after the camp ended, the athlete reported to his athletic trainers with the chief complaint of severe bilateral leg pain in his quadriceps. Two days after the initial assessment, he was admitted to the hospital where he was diagnosed based on creatine kinase (CK) levels that peaked at 146,000 IU/L. He was hospitalized for six days where he received intravenous normal saline for rehydration, and his CK levels were assessed daily. If that wasn’t enough, the 16-year old mentioned he drank less than a half-cup of water during his training, due to infrequent water breaks. His discharge instructions consisted of limited walking, no cardiovascular exercise, and no weight training exercises (even with upper body exercises) to avoid added muscle damage. He was provided a handout with instructions for gentle stretching, emphasizing hip and knee flexion within his pain-free range of motion. He was sent home with a wheelchair and crutches. Because transportation at school would be difficult, particularly because there were no stairs or elevators, he completed his class work at home. The athlete did not return to school for two months. Within three months, he was back to normal and fully recovered (5).
Shockingly, a case involving a 12-year-old boy described his participation in an indoor physical education class during which he was required to perform excessive (250 repetitive squat jumps as punishment for talking in class). The boy reported intense muscle soreness in his thighs and dark urine two days post-exercise, and his parents brought him to the emergency room. He was hospitalized with serum CK rising to 244,006 IU/L at 4 days post-exercise and was diagnosed with my condition (3).
Most Extreme Cases (2002-2013)
What can you do?
Currently, there are no specific treatments available for patients with my condition. The primary objective during treatment is to preserve and prevent further ailment and deleterious effects of my condition to your body. While there are no clear guidelines for treatment, it’s recommended those with my disease should seek hospitalization with highly increased creatine kinase activity, decreased creatinine clearance, myoglobinuria, metabolic abnormalities, or signs of compartment syndrome.
The laboratory diagnosis of my condition is almost always based on elevation of creatine kinase activity to more than five times the upper limits of normal (10). However, there are baseline differences considering people are high, low or no responders. CK activities after physical exercise can vary widely between individuals and are associated with gender, race, and fitness, with normal values not clearly defined either.
Personal trainers, strength coaches, athletic trainers, personal trainers, and physical education teachers, should identify any young or older individuals reporting significant red-flag symptoms of me via muscular aches, muscle weakness, and cola-colored (or slight variations of this color) urine that develops within 12–36 hours after the damaging training session(s). Individuals should be evaluated and risk stratified as high or low risk prior to returning to activity. Stressful environmental conditions may lead to dehydration and can lead to my condition, particularly when the individual is not accustomed to the extreme exercise intensity.
Bottom Line: I’ve always been here and have been around for decades. Some people and/or certain training protocols just activate me more so than others, even though I’m always alive and don’t always stay dormant.
References
1. Baird MF, Graham SM, Baker JS, and Bickerstaff GF. Creatine-kinase- and exercise-related muscle damage implications for muscle performance and recovery. J Nutr Metab 2012, 2012.
2. Brentano MA and Martins Kruel LF. A review on strength exercise-induced muscle damage: applications, adaptation mechanisms and limitations. J Sports Med Phys Fitness 51: 1-10, 2011.
3. Clarkson PM. Case report of exertional rhabdomyolysis in a 12-year-old boy. Med Sci Sports Exerc 38: 197-200, 2006.
4. Clarkson PM, Nosaka K, and Braun B. Muscle function after exercise-induced muscle damage and rapid adaptation. Med Sci Sports Exerc 24: 512-520, 1992.
5. Cleary MA, Sadowski KA, Lee SY, Miller GL, and Nichols AW. Exertional rhabdomyolysis in an adolescent athlete during preseason conditioning: a perfect storm. J Strength Cond Res 25, 2011.
6. Giannoglou GD, Chatzizisis YS, and Misirli G. The syndrome of rhabdomyolysis: Pathophysiology and diagnosis. European journal of internal medicine 18: 90-100, 2007.
7. Kahanov L, Eberman LE, Wasik M, and Alvey T. Exertional rhabdomyolysis in a collegiate american football player after preventive cold-water immersion: a case report. J Athl Train 47, 2012.
8. Knochel JP. Catastrophic medical events with exhaustive exercise: "white collar rhabdomyolysis". Kidney Int 38: 709-719, 1990.
9. Landau ME, Kenney K, Deuster P, and Campbell W. Exertional rhabdomyolysis: a clinical review with a focus on genetic influences. Journal of clinical neuromuscular disease 13, 2012.
10. Melli G, Chaudhry V, and Cornblath DR. Rhabdomyolysis: an evaluation of 475 hospitalized patients. Medicine 84: 2005.
11. Moeckel-Cole SA and Clarkson PM. Rhabdomyolysis in a collegiate football player. J Strength Cond Res 23: 1055-1059, 2009.
12. O'Connor FG, Brennan FH, Jr., Campbell W, Heled Y, and Deuster P. Return to physical activity after exertional rhabdomyolysis. Curr Sports Med Rep 7: 328-331, 2008.
13. Pearcey GE, Bradbury-Squires DJ, Power KE, Behm DG, and Button DC. Exertional rhabdomyolysis in an acutely detrained athlete/exercise physiology professor. Clin J Sport Med 23: 496-498, 2013.
14. Sauret JM, Marinides G, and Wang GK. Rhabdomyolysis. American family physician 65: 907-912, 2002.
15. Sayers SP and Clarkson PM. Exercise-induced rhabdomyolysis. Curr Sports Med Rep 1: 59-60, 2002.
16. Springer BL and Clarkson PM. Two cases of exertional rhabdomyolysis precipitated by personal trainers. Med Sci Sports Exerc 35: 1499-1502, 2003.
17. Vanholder R, Sever MS, Erek E, and Lameire N. Rhabdomyolysis. J Am Soc Nephrol 11: 2000.