
Introduction
Stress is a buzzword that garners attention but very little follow-through regarding effective management. According to a 2014 poll, 25% of Americans reported experiencing high stress, and roughly 50% claimed they had experienced a significant stressful life event within the past year (1). Given the steep rise in mental health occurrences, I would speculate that these figures likely underreport the prevalence of distress in Canada and the US. Especially considering the recent COVID-19 endemic and the ensuing economic recession, the rates of depression, stress, anxiety, suicide, etc, have increased considerably.
The objective of this article is to explore stress, discussing mechanisms, physiological responses and adaptations, behavioral responses, differentiating chronic stress from productive stress and building resilience. Finally, we will cover the various approaches which can be used to increase stress tolerance and resilience, and reduce and effectively manage stress to (hopefully) live a healthier, happier, and more productive life.
Understanding the Stress Response
Homeostasis is the body's proclivity to maintain a state of equilibrium. For instance, if our core temperature elevates or decreases suddenly, various physiological and behavioral mechanisms kick in to bring our body's temperature back within a stable range (2).
Allostasis is the process by which the body responds to a stressor to regain homeostasis. This brings up the subject of stress tolerance and adaptive thresholds. Each individual will have their own adaptive threshold. You can think of this as similar to lifting weights. Some individuals can simply lift more weight and tolerate greater workloads. While others given the same workload may not be able to recover and eventually burn out or get injured.
Resilience refers to how effectively your system returns to baseline (3). Thus we see differences in stress tolerance as well as individual ability to buffer or otherwise effectively manage stress that are influenced by both genetic and environmental variables.
RECENT: Build Your Ruck Without Breaking Your Body
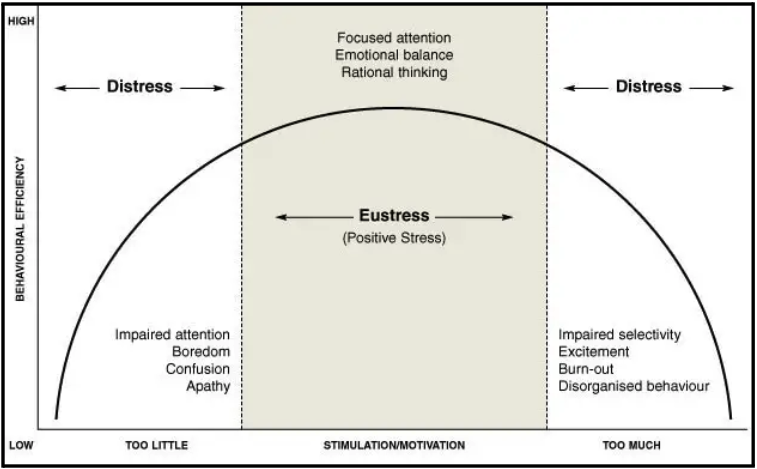
Eustress can be thought of as a stressor that falls within the productive threshold of adaptation. Thus, an individual experiencing a stressor of this sort will likely be able to adapt and become more resilient in the future. Eustress is thought to be short-term, falls within the adaptive threshold of the individual, improves performance, and motivates and focuses energy. Think of the heightened level of stress/anxiety/nervousness during a competition. This is productive and prepares you for optimal performance.
Distress can be considered a stressor that exceeds an individual's current adaptive threshold and may become a noxious stimulus. This is counterproductive, often causing anxiety, unpleasant feelings, decreased performance, exceeds current adaptive capacity, and can lead to psychological and physiological harm. See the image below for a visual representation.
As you can see in the image, too little stress can be bad. During resistance training, we act against an external force to overcome it. This leads to physiological adaptations that can make us stronger, faster, more muscular, explosive, and ultimately more resilient. Without engaging our bodies physically, we become weak, frail, and more prone to disease. Our body and mind respond similarly to stress. Without a certain amount of resistance (stress), we become frail and more susceptible to various environmental disturbances (the left side of the chart).
Conversely, too much stress pushes us into a state of dysfunction (right side of the chart). The objective, then, is twofold. The first would be to manage stressors to stay within the productive threshold of adaptation (middle of the chart). The second would be to slowly expand the range of tolerance over time to become more resilient.
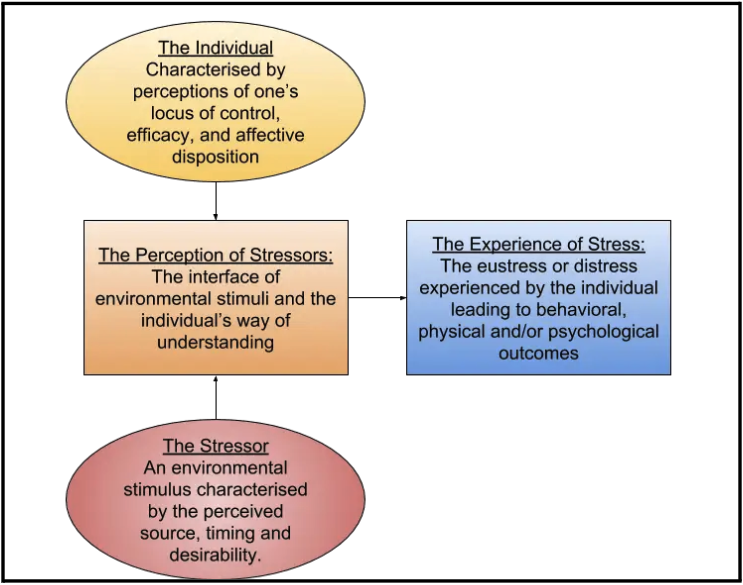
An important aspect of the response to stress is the individual's starting perception of stress. Control theory proposes that an individual's sense of control over their environment can buffer the negative effects of stress (4). This leads to a related topic, "locus of control," which refers to an individual's belief that they have agency over their lives and the events affecting them (5). You can have an internal or external locus. Individuals with a high internal locus of control believe that they have agency over their lives and events are primarily influenced by their actions and behaviors. Individuals with a high external locus of control believe they have little control over their lives and are essentially at the mercy of uncontrollable external forces.
One paper found, "Those with a more internal locus of control tend to feel happier, more free, and less stress. They also enjoy better health (likely because they experience less damaging chronic stress that can come from feeling powerless) and are more satisfied with life in general. Those with an external locus of control are more susceptible to depression and other health problems and tend to keep themselves in situations where they will experience additional stress—feeling powerless to change their circumstances, which adds to their stress." (6). The image below visually represents how an individual's perspective can shape their psychological and physiological response to stress.
Although an internal locus of control is generally thought to be better, there is also a risk of internalizing things outside your control. Considering how much of our lives are based on chance, claiming ownership of things outside your control can be problematic. Events that don't align as planned can damage a sense of self-efficacy. According to Bandura (1977), self-efficacy is an individual's belief in his or her capacity to execute behaviors necessary to produce specific performance attainments (7). Thus if you direct your efforts toward tasks that do not affect the outcome, it can give you a false sense of inadequacy. However, a more accurate characterization would be the misappropriation of resources and attention.
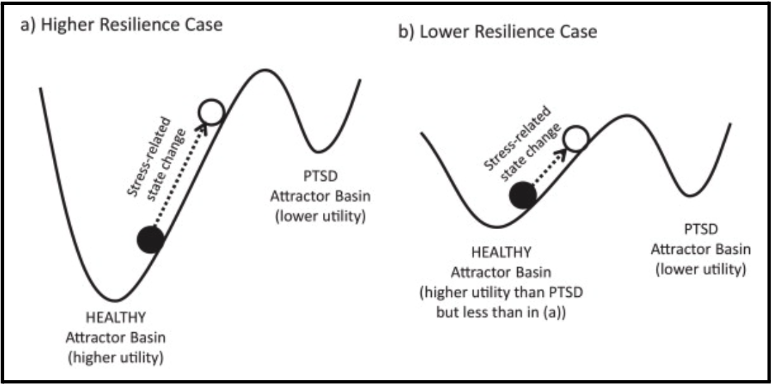
A 1973 paper by Holling et al. discusses the stress response in terms of being in a high-utility vs. low-utility state. Stress is dose-dependent. Therefore a high-dose stressor such as disease, divorce, death of a loved one, etc., can elicit a stress-related state change into what's known as a lower utility state. In this state, your functional capabilities are impaired. This brings up another important point regarding acute vs. chronic stressors. An acute stressor is a short-term stress, such as a fight with your significant other or a car accident. Chronic stress is a long-term stressor, such as a divorce that follows a fight with your significant other or dealing with injury or inability to work due to a car accident.
Both acute and chronic stressors exist on a severity scale as well. An acute stressor can be minor or significant enough to cause trauma and shift you into a state of chronic stress. The individual's baseline resilience, the magnitude of the stressor, and their perception of the experience largely dictate whether they will remain in the "higher utility" basin or shift into a "lower utility basin," as depicted below.
An individual who experiences chronic stress may be stuck in a state of fight or flight, as experienced by individuals with PTSD. Stress levels are chronically elevated in this state, and the threshold for recurrent episodes may be lowered due to this gridlocked psychological and physiological state.
Stress, Physiology, and Psychology
The primary elements of the stress reaction system are the hypothalamic-pituitary-adrenal axis (HPA axis) and the autonomic nervous system (ANS), which then communicate with the central nervous system (CNS) and various other systems within the body to mount a response (8). Acute stress elicits changes in behavior, physiology, and psychology. Some of which are changes in cardiovascular tone, respiration, and heart rate. Substrates and other resources are redirected from systems deemed temporarily unimportant (i.e., digestion, reproduction, immunity) to sites in the body where they're needed most, such as muscles. The image below highlights some of the behavioral and physical adaptations that occur during stress.
| Behavioral Adaptation |
| Adaptive redirection of behavior |
| Increased arousal and alertness |
| Increased cognition, vigilance and focused attention |
| Suppression of feeding behavior |
| Suppression of reproductive behavior |
| Inhibition of gastric motility; stimulation of colonic motility |
| Containment of the stress response |
| Physical Adaptation |
| Adaptive redirection of energy |
| Oxygen and nutrients directed to the central nervous system and stressed body site(s) |
| Altered cardiovascular tone; increased blood pressure and heart rate |
| Increased respiratory rate |
| Increased gluconeogenesis and lipolysis |
| Detoxification from toxic products |
| Inhibition of reproductive and growth axes |
| Containment of the stress response |
| Containment of the inflammatory/immune response |
As you can see from the list above, many of these adaptations are beneficial in a potentially dangerous encounter. However, when stress is chronically elevated, it's clear that these responses can become problematic and even predispose an individual to various disease states. As mentioned previously, awareness of the stressor in itself may independently be a stressor, sometimes called "stress awareness." If you've ever been in bed and worried about falling asleep, then worried about the fact that you're worried about falling asleep, you've experienced stress awareness.
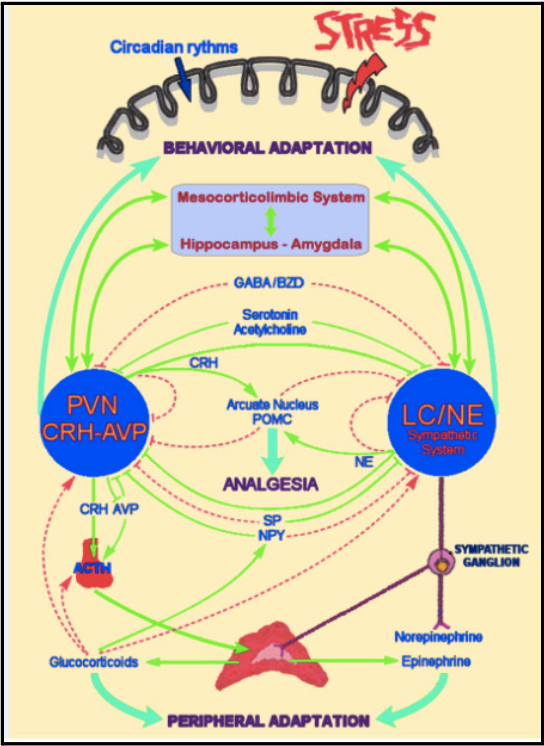
As a 2020 paper by Tsigos et al. noted, "The stress system is tightly interconnected with all the major endocrine axes, including the reproductive, growth, and thyroid axis. This ensures that the activity of the endocrine system is rapidly regulated in a coordinated and precise way to serve the adaptive stress response and maximize the chances of survival against the imposed stressor(s). As such, the central components of the stress system are located in the hypothalamus and the brainstem and include the parvocellular corticotropin-releasing hormone (CRH) and arginine-vasopressin (AVP) neurons of the paraventricular nuclei (PVN) of the hypothalamus, and the CRH neurons of the paragigantocellular and parabranchial nuclei of the medulla, as well as the locus coeruleus (LC) and other catecholaminergic, norepinephrine (NE)-synthesizing cell groups of the medulla and pons (central sympathetic nervous system)" (8)(9)(10)(11)(12). The image below depicts their interconnected relationship.
Glucocrticoids are steroid hormones produced via the adrenal glands. They play a meaningful role in the metabolism of glucose, carbohydrates, and fat (13). They also help regulate the HPA axis. Research also shows pulsatility is a driving factor in determining the HPA axis's response to stress and the termination of the stress response (14)(15). As stated in a 2010 paper, "Glucocorticoids synthesized in the adrenal cortex in response to adrenocorticotropic hormone (ACTH) stimulate gluconeogenesis to provide energy for the "flight or fight" response. The response to stress combines suppressive and stimulating actions of glucocorticoids for the ultimate goal of preservation of self" (16).
It's been shown that physiological (injury, disease, etc.) and psychological stressors (anxiety, depression, etc.) trigger an increase in glucocorticoids that suppress various reproductive functions along the hypothalamo-pituitary-gonadal (HPG) axis (17)(18). For women, distress can disrupt regular physiological function causing delayed ovulation or irregular and even missed periods. For males, it can lead to a reduction in reproductive function and even erectile dysfunction.
Cardiovascular health is another major consideration when discussing stress. Some research has estimated psychological stress increases risk of coronary heart disease by roughly 40-60% (19)(20). Other research has found extreme stress during childhood was associated with an even greater risk than stress in adulthood (21). A 2022 paper found "increased sympathetic nervous system activity, parasympathetic withdrawal, increased circulating catecholamines (e.g., epinephrine, norepinephrine), increased cortisol levels, increased plasma pro-inflammatory cytokines, and immune system activation. In addition to these systemic processes, stress perception also results in the activation of preganglionic sympathetic neurons in the spinal cord, which via prevertebral or paravertebral ganglia directly innervate end organs, including the heart.13 Resultant hemodynamic changes with mental stress include increased heart rate, blood pressure, systemic vascular resistance, and cardiac output" (22).
Suffice it to say, various forms of distress are associated with an increased incidence of acute cardiac events. Researchers have reported acute psychological stress can lead to myocardial ischemia and infarction via prothrombotic and pre-inflammatory effects, platelet activation, aggregability, and pro-inflammatory activity. We see increases in blood viscosity, pro-inflammatory cytokines, and various other related factors.
Stress also impacts eating behavior by influencing satiety signaling in the hypothalamus. Some individuals report reduced appetite, nausea, and a general loss of motivation to eat during periods of high stress. Others experience dietary disinhibition followed by binging behavior. This behavior is characterized by a strong compulsion to eat often accompanied by a fast initial rate of eating. There is often a delay or absence of satiety perception, contributing to the faster food consumption rate (23)(24).
Chronic stress has also been shown to disrupt natural sleep rhythm. Since sleep restriction is associated with increased caloric consumption, decreased dietary restraint, and higher levels of adiposity, there is also a clear risk of stress leading to sleep restriction, which can lead to further impairment of normalized eating habits. Dysregulation of the biological circadian rhythm due to stress can create a negative feedback loop where stress disrupts sleep, which increases stress, and so on. If sleep restriction is left unchecked, it can increase the risk of various disease states, such as metabolic and cardiovascular disorders (25)(26)(27)(28)(29).
Stress can even impair your ability to progress as a lifter. One paper aimed to determine the effects of chronic stress on muscular function and things like perceived fatigue, soreness, energy, etc. The study design was as follows "Undergraduate resistance training students (n = 31; age, 20.26 ± 1.34 years) completed the Perceived Stress Scale and the Undergraduate Stress Questionnaire, a measure of life event stress.
At a later visit, they performed an acute heavy-resistance exercise protocol (10 repetition maximum [RM] leg press test plus 6 sets: 80-100% of 10RM). Maximal isometric force (MIF), perceived energy, fatigue, and soreness were assessed in approximately 24-hour intervals after exercise." (30). During the initial testing, no significant differences were found between groups in any measured parameters (1RM strength, cycling power, jump height, etc.). Researchers found the recovery of the high-stress group was substantially slower compared to the low stress cohort. This can have major implications considering fatigue and adaptations are cumulative. Thus, high stress increases the total allostatic burden and burns through more of your adaptive resources.
It's also been shown that chronic stress can lead to atrophy of brain mass, structural changes that negatively impact cognition and memory, long-term effects on the nervous system, and various other pathologies (31)(32)(33)(34)(35)(36). A 1999 paper by Bremner found "Patients with posttraumatic stress disorder (PTSD) from Vietnam combat and childhood abuse had deficits on neuropsychological measures that have been validated as probes of hippocampal function. In addition, magnetic resonance imaging (MRI) showed a reduction in volume of the hippocampus in both combat veterans and victims of childhood abuse. In combat veterans, hippocampal volume reduction was correlated with deficits in verbal memory on neuropsychological testing.
These studies introduce the possibility that experiences in the form of traumatic stressors can have long-term effects on the structure and function of the brain." (37). Researchers have also found an inverse relationship between cortisol and memory, such that elevated cortisol levels due to chronic stress were associated with impaired memory and improved once plasma cortisol levels returned to baseline (38)(39)(40). Interestingly enough, stress's impact on memory largely depends on the dose and duration of the exposure as well as the context. If you decide to cram for a test, you may temporarily experience an enhanced memory. But it may have the reverse effect if you're stressing over the test and doubting your ability. So as mentioned previously, the impact of stress on memory is contingent on the various factors mentioned earlier in this paragraph.
How to Protect Yourself From Stress
At this point, we've taken a comprehensive look at stress. We've highlighted that stress is functional, but if left unchecked eustress can quickly turn into distress. There are two ways you can protect yourself from stress. The first is to limit your exposure to stressors that far exceed your functional capacity to adapt. The second is to increase your stress resilience by elevating your allostatic tolerance. Or you can use a combination of the two. In this section, we'll discuss various interventions and their impact on stress reduction, increasing stress resilience, or both.
Saunas
Saunas can enable individuals to relax. A sit in the sauna leads to an associated increase in body temperature. This leads to improved blood flow to skin and organs, increased cardiac output, reduction in blood pressure, and increased heart rate. One paper found "positive alteration in levels of circulating lipids, improvement in glucose metabolism, improved arterial stiffness, arterial compliance, and intima media thickness, and improvement in the cardiorespiratory system, as well as CV function.
Some early evidence indicates that sauna bathing improves cardiac autonomic nervous system balance, leading to an increase in vagal tone and a decrease in sympathetic tone, with positive modulations in heart rate variability during the recovery from sauna." (41). Hormesis is an adaptive response to stress (42). During heat exposure, your body releases endorphins and dynorphins. Everyone is familiar with endorphins, often colloquially referred to as the happy hormone. Dynorphin is a neuropeptide involved in pain, addiction, and mood regulation. Dynorphins initially cause acute stress, but this is a hormetic response that improves mood and a general sense of well-being.
Regularly using saunas has been shown to decrease cortisol levels, enhance activation of heat dependent mechanisms called heat shock proteins, and signal DNA repair (43)(44). Saunas have also been shown to benefit cardiovascular health. Based on the available data, a good general guideline is to get a total of 60 minutes of sauna time per week. This guideline should be broken up into intervals of 5-20 minutes interspersed throughout the week. A good starting point would be 3 x 20-minute sessions or 4 x 15-minute sessions. The sauna temperature should be 80-100 ℃ (176-212 ℉). Saunas may not be appropriate for everyone, including those with a particular health condition that's contraindicated here. So seek advice from a qualified medical professional before implementing any thermal therapy intervention.
Socialization and Connection
Humans are social creatures. We have evolved to rely on others for protection, support, reproduction, and connection. Social connection has been shown to decrease feelings of loneliness, depression, and anxiety while enhancing feelings of security, belonging, and happiness. A 2011 paper by Umberson et al. found defined various forms of social connection, "Social integration refers to overall level of involvement with informal social relationships, such as having a spouse, and with formal social relationships, such as those with religious institutions and volunteer organizations. Quality of relationships includes positive aspects of relationships, such as emotional support provided by significant others, and strained aspects of relationships, such as conflict and stress. Social networks refer to the web of social relationships surrounding an individual, in particular, structural features, such as the type and strength of each social relationship. Each of these aspects of social relationships affects health." (45).
Prospective studies of mortality have consistently shown that individuals with the lowest social involvement have a higher risk of death compared with those who have stronger social ties (46)(47). Social connection also appears to have a protective effect on mortality in individuals with existing health conditions, with one paper finding social isolation among individuals with coronary artery disease resulted in a 2.4 times increase in risk of cardiac death compared to their socially connected peers (48). These findings held stable when accounting for confounding variables such as socioeconomic status, health behaviors, and other related variables. The way by which social connection positively impacts physical and mental health is complex. But it appears to enhance health-based behaviors, provide a sense of meaning and fulfillment, entertainment, a sense of connectedness, improve depressive and anxiogenic symptoms and enhance general well-being.
[I'll take a moment to go off on a bit of a tangent. We are much more connected with social media, video calling, texting, etc. But this kind of connection is often shallow and gives the impression we are deeply connected. But it is no substitute for actual in-person connection. I'd highly recommend "Lost Connections" by Johan Hari. It's a fantastic read (and also available as an audiobook), very insightful, and does an excellent job diving into depression, anxiety, and how various physiological and psychological illnesses are related to lack of social connection.]
Due to significant variability in circumstance, personality, social network, etc., developing an "evidence-based" recommendation for the dose and type of social connection one should strive to maintain is difficult. Suffice it to say people have different needs, so this will be largely individually driven. Personally, I've always been a workaholic. I'd spend hours reading research daily, writing reviews, watching lectures, etc. I have many friends but would never make time for any of them. I was a recluse.
Roughly one year ago, I received some news about my health which changed my life. Since then, I have begun to prioritize the people in my life: my friends, family, and close personal relationships. Honestly, it's been one of the most impactful decisions I've ever made on my quality of life and sense of fulfillment.
Initially, I let the pendulum swing too far in the opposite direction. I was going out to see friends every evening. I was having a blast, but after a few weeks, I realized my personal goals were on the back burner. I realized that although I'm happy now, I wouldn't be for much longer if my health started to slide, my business stopped generating revenue, and my goals and aspirations fell to the wayside. So I reigned it in, and now I've found a balance where I still spend ample time with others, but not at the expense of my goals and things that are deeply meaningful to me.
What might that balance look like for you? I have no idea, but like me, you'll likely have to work to find the right balance.
Sleep and Restoration
Sleep is a critical element of high performance. Less discussed is the effect of sleep restriction on stress. Research has found that just a few nights of sleep restriction can significantly affect appetite regulation, neuroendocrine stress response, increased sympathetic tone, and cortisol (49). Chronic sleep deprivation can increase risk of cardiovascular disease, metabolic disorders like diabetes, and all cause mortality (50). Deteriorating health, poor mood, low energy, and general lethargy can also increase stress due to an awareness of one's declining health. Stress tolerance also appears to be blunted in a sleep-restricted state, making you more vulnerable to homeostatic disruption. Sleep is strongly linked to the HPA axis and various mechanisms of the stress response. It's a reciprocal relationship whereby stress can impair sleep quality and duration, increasing stress sensitivity and disrupting the natural circadian rhythm.
Connecting with Nature
Connecting with nature may sound like new-age fluff, but I assure you exposure to nature is necessary for health and well-being. One paper looked at the effects of visiting an urban forest on headaches, stress level, and their subjective sense of balance prior to and after visiting the park. Researchers found, "In terms of the average improvements over pre-visit levels, the overall recovery rate for stress was 87%, and the reduction in headache was 52% of the possible enhancement on a five-point scale." (51).
The biophilia hypothesis claims that humans have evolved in nature and are drawn to it (52). By extension, there are two primary rationales for this. The first is the Attention Restoration Theory which posits that the mental fatigue of daily life is associated with a reduced capacity to focus attention, and direct exposure to nature helps restore this functionality (53). The second rationale is the Stress Reduction Theory which posits spending time in nature activates the parasympathetic nervous system and downregulates stress (54)(55).
A 2018 systematic review looked at various forms of nature exposure and the associated effects on stress. It included nature viewing, outdoor walks, outdoor exercise, and gardening. Researchers found heart rate and blood pressure improved, and various self-reported measures also improved, indicating that spending time outdoors in nature (specifically green spaces) can reduce stress and improve health to a meaningful degree (56).
Another paper found "evidence for associations between nature exposure and improved cognitive function, brain activity, blood pressure, mental health, physical activity, and sleep. Results from experimental studies provide evidence of protective effects of exposure to natural environments on mental health outcomes and cognitive function. Cross-sectional observational studies provide evidence of positive associations between nature exposure and increased levels of physical activity and decreased risk of cardiovascular disease" (57). Greater access to green spaces has been associated with mental well-being, improved cognition, lower psychological distress, better mood, and higher quality of life (58)(59)(60). These benefits have a compounding effect when combined with physical activity (i.e., jogging, yoga, rock climbing, etc.) or social connection (i.e., playing team sports, enjoying social time with friends and family, etc.).
Based on the available evidence, it's clear that spending time in nature can be restorative and positively impact mental well-being and stress reduction. All of the clients I coach have a step target. A step target is important for baseline cardiovascular health, but also psychological well-being. There is research showing breaking up sedentary time has a positive impact on health. I often advocate going for multiple short walks per day (depending on the circumstances and constraints of the individual) to break up the monotony of work or other tasks and aid in digestion post-consumption. Try taking your next stroll in nature! Ultimately, find something that fits your lifestyle and routine.
Proper Nutrition
Like many other facets, nutrition has a somewhat reciprocal relationship with stress. Poor nutrition habits, if sustained over a long enough period, can reduce energy, obesity, and various metabolic conditions. Along this spectrum, your stress levels can also be impacted, which can reinforce delirious eating behavior. One paper looking at highly stressed caregivers found "Caregivers also had stable levels of poor metabolic functioning and greater reward-based eating across both time points, and evidenced increased abdominal fat prospectively (all ps ≤.05), independent of change in BMI." (61). Chronic stress can change eating patterns. It can be especially problematic, as seen in individuals who use food as a functional coping mechanism via overconsumption of calorically dense, highly palatable foods (62). Over time this behavior can become a conditioned response to psychological or emotional distress and, if left unchecked, may even develop into a clinically recognized eating disorder.
Good nutrition habits can lead to higher, more stable energy levels, healthy body fat levels, improved sleep, increased productivity, better adaptive response to training, and increased adaptive reserves for buffering stress. The opposite is also true, so maintaining healthy eating habits is important for longevity and effective stress management.
MORE: The Ultimate Guide to Designing a Muscle-Building Diet
Physical Exercise
Volitional exercise can reduce obesity, mediate depression, anxiety/stress, and improve overall health markers. It can significantly affect stress reduction since the reduction or absence of disease or ill health can remove a significant burden. Various forms of physical activity increase regional cerebral blood flow, cognition, stress resilience, cardiovascular health, learning, and neurogenesis in the hippocampus and prefrontal cortex (63). Exercise mediates many internal mechanisms that regulate stress.
As noted in a 2010 paper by Esch et al., "There seems to exist a common neurobiological mechanism, i.e., limbic autoregulation, that involves dopamine, morphine, and other endogenous signaling molecules, e.g., other opioid receptor agonists, endocannabinoids, oxytocin or serotonin, many of which act via NO release, and this share seems to be of critical importance for the self-regulation and management of stress: stress management is an endogenous potential" (64). Aerobic exercise appears to be very effective in this regard. However, a combination of aerobic and resistance-based exercise is recommended.
Exercise induces stress reduction through various pathways. As mentioned previously, if combined with social connection (i.e., training with friends or lifting partners) and being in nature (i.e., going for a trail run), the beneficial effect on stress reduction compounds. Exercise has a clear impact on physical and psychological well-being, often leading to an improvement in strength, physical health, immune robustness, stress reduction, depression, anxiety, and various other mood disorders (63). Exercise prescriptions can vary depending on individual context.
Since the majority of readers here will already have experience in resistance training, I don't think it's necessary to give specific exercise prescriptions since there may be significant heterogeneity. However, a good rule of thumb is to get two to three resistance training sessions and two to three aerobic training sessions per week. You can do both on the same days, alternate days, or any other approach you deem appropriate.
More important than the specific dose is to get started and refine the approach to what works best for you, your goals, and your situation. Then continue to iterate as time goes on. If you'd like a more in-depth discussion on designing an individualized program, I recorded a comprehensive video on how to design a strength training program.
Breathwork
Although there is an overlap between breathwork and meditation, they are distinctly different. A 2023 study by Balban et al. found, "Using a mixed-effects model, we show that breathwork, especially the exhale-focused cyclic sighing, produces greater improvement in mood (p < 0.05) and reduction in respiratory rate (p < 0.05) compared with mindfulness meditation. Daily 5-min cyclic sighing has promise as an effective stress management exercise" (65). That's not to suggest meditation or mindfulness doesn't have this effect. Rather, breathwork is valuable independent of the specific meditative modality. Other research has found that yoga positively affects circulating cortisol and inflammatory markers like C-reactive protein, interlukin-1, interlukin 6, and other cytokines (66). Although some beneficial effects are likely bolstered with the additional physical activity in yoga, breathwork still plays a meaningful role in stress reduction and mitigation.
One paper titled "Effect of breathwork on stress and mental health: A meta-analysis of randomised-controlled trials" aimed to evaluate the efficacy of breathwork and its effects on stress. The authors did note a moderate risk of bias from the reviewed RCT's, however the findings suggest that breathwork may be an effective tool in moderating stress and mental health (67). Although the mention of bias should caution individuals to be skeptical when evaluating claims, it doesn't mean they should be dismissed. Especially given the prevalence of breathwork in various clinical settings, meditative practices, and cultures, it seems highly unlikely that its effects on stress and mental health are insignificant. Below is a breathwork practice that I've found to be highly effective called box breathing:
Box Breathing
- Step 1: Breathe in through your nose for a count of four.
- Step 2: Hold your breath for a count of four.
- Step 3: Exhale through your mouth for a count of four.
- Step 4: Hold at the end of your exhalation for a count of four.
Some people find step four very difficult. If you find it causes some anxiety, skip Step 4 and cycle through Steps 1-3 for just a few minutes. Working up to five minutes of box breathing is much more difficult than you might think. So set a manageable target for yourself at the onset. Start small and slowly progress from there. If you want to learn more about breathwork, I recorded a podcast with Brian Mackenzie, one of the leading experts on the subject. We discuss breathing, stress, athletic performance, and specific breathwork protocols to reduce stress and enhance recovery.
Closing Remarks
Being chronically stressed sucks. It's something I've dealt with through my entire adult life. I was diagnosed with complex dissociative PTSD. Essentially this means I'm in a perpetual state of high stress fight or flight. I know people talk about normalizing mental health issues, but if I'm being honest, most of it is just empty gestures. I've had several people express a similar experience when they tried to speak about their difficulties. Stress has many root causes, and not everyone experiencing stress has a mental health problem. But many do, and I'm not qualified to give prescriptions to anyone battling mental health issues. That being said, it is a subject close to my heart, and I wanted to offer some resources for anyone struggling.
The first resource is an online therapy through Better Help. Their mission is "Making professional therapy accessible, affordable, and convenient—so anyone who struggles with life's challenges can get help anytime and anywhere." I've used their services and found them to be quite helpful. I've also referred many others to them who have found a similar benefit.
The second resource is a psychotherapist named Seerut K. Chawla. I found her on Instagram and was repeatedly impressed by her perspective, and I found many of her insights applicable to my own situation. She is direct, no-nonsense, and has an incredibly unique perspective on therapy and mental health. I have never worked with her, but I have consumed a ton of her content, and if I were in a place where I needed to hire a therapist, I would 100% reach out to her.
To clarify, I have no affiliation, nor do I receive any incentives, financial or otherwise, from either of these companies. I genuinely think they're great resources.
References
- Blendon, R., G. Steel Fisher, K. Weldon, J. Benson, M. Brule, F. Mann, C. Miller, and A. Kramer. "The burden of stress in America." NPR/Robert Wood Johnson Foundation Harvard School of Public Health (2014): 1-12.
- Chrousos GP. Stress and disorders of the stress system. Nat Rev Endocrinol. 2009 Jul;5(7):374-81. doi: 10.1038/nrendo.2009.106. Epub 2009 Jun 2. PMID: 19488073.
- Hollings, C. S. (1973). Resilience and stability of Ecological Systems | annual review of ... Resilience and Stability of Ecological Systems. https://www.annualreviews.org/doi/10.1146/annurev.es.04.110173.000245
- Spector, P. E., & Goh, A. (2001). The role of emotions in the occupational stress process. In P. L. Perrewé & D. C. Ganster (Eds.), Exploring theoretical mechanisms and perspectives (pp. 195–232). Elsevier Science/JAI Press. https://doi.org/10.1016/S1479-3555(01)01013-7
- Lefcourt HM. Internal versus external control of reinforcement: a review. Psychol Bull. 1966 Apr;65(4):206-20. doi: 10.1037/h0023116. PMID: 5325292.
- Paranjpe, Vedavati. (2014). The Relationship between Locus of Control and Perceived Stress. Indian Journal of Mental Health(IJMH). 1. 64. 10.30877/IJMH.1.1.2014.64-70.
- Bandura, A. (1997). Self-efficacy: The exercise of control. W H Freeman/Times Books/ Henry Holt & Co.
- Tsigos C, Kyrou I, Kassi E, et al. Stress: Endocrine Physiology and Pathophysiology. [Updated 2020 Oct 17]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK278995/
- Chrousos GP. Stress and disorders of the stress system. Nat Rev Endocrinol. 2009 Jul;5(7):374-81. doi: 10.1038/nrendo.2009.106. Epub 2009 Jun 2. PMID: 19488073.
- Chrousos GP, Gold PW. The concepts of stress and stress system disorders. Overview of physical and behavioral homeostasis. JAMA. 1992 Mar 4;267(9):1244-52. Erratum in: JAMA 1992 Jul 8;268(2):200. PMID: 1538563.
- Chrousos GP. Regulation and dysregulation of the hypothalamic-pituitary-adrenal axis. The corticotropin-releasing hormone perspective. Endocrinol Metab Clin North Am. 1992 Dec;21(4):833-58. PMID: 1486878.
- Tsigos C, Chrousos GP. Physiology of the hypothalamic-pituitary-adrenal axis in health and dysregulation in psychiatric and autoimmune disorders. Endocrinol Metab Clin North Am. 1994 Sep;23(3):451-66. PMID: 7805648.
- Chourpiliadis C, Aeddula NR. Physiology, Glucocorticoids. [Updated 2022 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560897/
- Lightman SL, Wiles CC, Atkinson HC, Henley DE, Russell GM, Leendertz JA, McKenna MA, Spiga F, Wood SA, Conway-Campbell BL. The significance of glucocorticoid pulsatility. Eur J Pharmacol. 2008 Apr 7;583(2-3):255-62. doi: 10.1016/j.ejphar.2007.11.073. Epub 2008 Feb 9. PMID: 18339373.
- Stavreva DA, Wiench M, John S, Conway-Campbell BL, McKenna MA, Pooley JR, Johnson TA, Voss TC, Lightman SL, Hager GL. Ultradian hormone stimulation induces glucocorticoid receptor-mediated pulses of gene transcription. Nat Cell Biol. 2009 Sep;11(9):1093-102. doi: 10.1038/ncb1922. Epub 2009 Aug 16. PMID: 19684579; PMCID: PMC6711162.
- Whirledge S, Cidlowski JA. Glucocorticoids, stress, and fertility. Minerva Endocrinol. 2010 Jun;35(2):109-25. PMID: 20595939; PMCID: PMC3547681.
- Rabin D, Gold PW, Margioris AN, Chrousos GP. Stress and reproduction: physiologic and pathophysiologic interactions between the stress and reproductive axes. Adv Exp Med Biol. 1988;245:377-87. doi: 10.1007/978-1-4899-2064-5_29. PMID: 3067563.
- Collu R, Gibb W, Ducharme JR. Effects of stress on the gonadal function. J Endocrinol Invest. 1984 Oct;7(5):529-37. doi: 10.1007/BF03348463. PMID: 6439774.
- Andrew Steptoe, A., & Mika Kivimäki, M. (2013). Stress and cardiovascular disease: An update on current knowledge. Stress and Cardiovascular Disease: An Update on Current Knowledge. https://www.annualreviews.org/doi/abs/10.1146/annurev-publhealth-031912-114452
- Steptoe, A., Kivimäki, M. Stress and cardiovascular disease. Nat Rev Cardiol 9, 360–370 (2012). https://doi.org/10.1038/nrcardio.2012.45
- Kivimäki, M., Steptoe, A. Effects of stress on the development and progression of cardiovascular disease. Nat Rev Cardiol 15, 215–229 (2018). https://doi.org/10.1038/nrcardio.2017.189
- Levine, G. N. (2022, March 9). Psychological stress and heart disease: Fact or folklore?. The American Journal of Medicine. https://www.sciencedirect.com/science/article/pii/S0002934322001371#bib0006
- Schulz S, Laessle RG. Stress-induced laboratory eating behavior in obese women with binge eating disorder. Appetite. 2012 Apr;58(2):457-61. doi: 10.1016/j.appet.2011.12.007. Epub 2011 Dec 16. PMID: 22200410.
- Spencer SJ, Tilbrook A. The glucocorticoid contribution to obesity. Stress. 2011 May;14(3):233-46. doi: 10.3109/10253890.2010.534831. Epub 2011 Feb 6. PMID: 21294656.
- Nicolaides NC, Charmandari E, Kino T, Chrousos GP. Stress-Related and Circadian Secretion and Target Tissue Actions of Glucocorticoids: Impact on Health. Front Endocrinol (Lausanne). 2017 Apr 28;8:70. doi: 10.3389/fendo.2017.00070. PMID: 28503165; PMCID: PMC5408025.
- Kassi EN, Chrousos GP. The central CLOCK system and the stress axis in health and disease. Hormones (Athens). 2013 Apr-Jun;12(2):172-91. doi: 10.14310/horm.2002.1402. PMID: 23933687.
- Chrousos GP, Kino T. Glucocorticoid action networks and complex psychiatric and/or somatic disorders. Stress. 2007 Jun;10(2):213-9. doi: 10.1080/10253890701292119. PMID: 17514590.
- Kino T, Chrousos GP. Acetylation-mediated epigenetic regulation of glucocorticoid receptor activity: circadian rhythm-associated alterations of glucocorticoid actions in target tissues. Mol Cell Endocrinol. 2011 Apr 10;336(1-2):23-30. doi: 10.1016/j.mce.2010.12.001. Epub 2010 Dec 10. PMID: 21146585; PMCID: PMC3057275.
- Kino T, Chrousos GP. Circadian CLOCK-mediated regulation of target-tissue sensitivity to glucocorticoids: implications for cardiometabolic diseases. Endocr Dev. 2011;20:116-126. doi: 10.1159/000321232. Epub 2010 Dec 16. PMID: 21164265; PMCID: PMC3163295.
- Stults-Kolehmainen MA, Bartholomew JB, Sinha R. Chronic psychological stress impairs recovery of muscular function and somatic sensations over a 96-hour period. J Strength Cond Res. 2014 Jul;28(7):2007-17. doi: 10.1519/JSC.0000000000000335. PMID: 24343323.
- Yaribeygi H, Panahi Y, Sahraei H, Johnston TP, Sahebkar A. The impact of stress on body function: A review. EXCLI J. 2017 Jul 21;16:1057-1072. doi: 10.17179/excli2017-480. PMID: 28900385; PMCID: PMC5579396.
- Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. 2009 Jun;10(6):434-45. doi: 10.1038/nrn2639. Epub 2009 Apr 29. PMID: 19401723.
- Reznikov LR, Grillo CA, Piroli GG, Pasumarthi RK, Reagan LP, Fadel J. Acute stress-mediated increases in extracellular glutamate levels in the rat amygdala: differential effects of antidepressant treatment. Eur J Neurosci. 2007 May;25(10):3109-14. doi: 10.1111/j.1460-9568.2007.05560.x. PMID: 17561824.
- https://www.ncbi.nlm.nih.gov/core/lw/2.0/html/tileshop_pmc/tileshop_pmc_inline.html?title=Click%20on%20image%20to%20zoom&p=PMC3&id=5579396_EXCLI-16-1057-t-001.jpg
- Lupien SJ, Lepage M. Stress, memory, and the hippocampus: can't live with it, can't live without it. Behav Brain Res. 2001 Dec 14;127(1-2):137-58. doi: 10.1016/s0166-4328(01)00361-8. PMID: 11718889.
- Bremner JD. Does stress damage the brain? Biol Psychiatry. 1999 Apr 1;45(7):797-805. doi: 10.1016/s0006-3223(99)00009-8. PMID: 10202566.
- Ling MH, Perry PJ, Tsuang MT. Side effects of corticosteroid therapy. Psychiatric aspects. Arch Gen Psychiatry. 1981 Apr;38(4):471-7. doi: 10.1001/archpsyc.1981.01780290105011. PMID: 7212976.
- Kirschbaum C, Wolf OT, May M, Wippich W, Hellhammer DH. Stress- and treatment-induced elevations of cortisol levels associated with impaired declarative memory in healthy adults. Life Sci. 1996;58(17):1475-83. doi: 10.1016/0024-3205(96)00118-x. PMID: 8622574.
- Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull. 2004 Jul;130(4):601-30. doi: 10.1037/0033-2909.130.4.601. PMID: 15250815; PMCID: PMC1361287.
- Laukkanen JA, Kunutsor SK. Is sauna bathing protective of sudden cardiac death? A review of the evidence. Prog Cardiovasc Dis. 2019 May-Jun;62(3):288-293. doi: 10.1016/j.pcad.2019.05.001. Epub 2019 May 16. PMID: 31102597.
- Mattson MP. Hormesis defined. Ageing Res Rev. 2008 Jan;7(1):1-7. doi: 10.1016/j.arr.2007.08.007. Epub 2007 Dec 5. PMID: 18162444; PMCID: PMC2248601.
- Podstawski R, Borysławski K, Pomianowski A, Krystkiewicz W, Żurek P. Endocrine Effects of Repeated Hot Thermal Stress and Cold Water Immersion in Young Adult Men. American Journal of Men’s Health. 2021;15(2). doi:10.1177/15579883211008339
- Iguchi, M., Littmann, A. E., Chang, S.-H., Wester, L. A., Knipper, J. S., & Shields, R. K. (2012, March 1). Heat stress and cardiovascular, hormonal, and heat shock proteins in humans. Allen Press. https://meridian.allenpress.com/jat/article/47/2/184/111268/Heat-Stress-and-Cardiovascular-Hormonal-and-Heat
- Umberson D, Montez JK. Social relationships and health: a flashpoint for health policy. J Health Soc Behav. 2010;51 Suppl(Suppl):S54-66. doi: 10.1177/0022146510383501. PMID: 20943583; PMCID: PMC3150158.
- House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988 Jul 29;241(4865):540-5. doi: 10.1126/science.3399889. PMID: 3399889.
- Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol. 1979 Feb;109(2):186-204. doi: 10.1093/oxfordjournals.aje.a112674. PMID: 425958.
- Brummett BH, Barefoot JC, Siegler IC, Clapp-Channing NE, Lytle BL, Bosworth HB, Williams RB Jr, Mark DB. Characteristics of socially isolated patients with coronary artery disease who are at elevated risk for mortality. Psychosom Med. 2001 Mar-Apr;63(2):267-72. doi: 10.1097/00006842-200103000-00010. PMID: 11292274.
- McEwen, B. S., & Karatsoreos, I. N. (2015, February 27). Sleep deprivation and circadian disruption: Stress, allostasis, and Allostatic Load. Sleep Medicine Clinics. https://www.sciencedirect.com/science/article/abs/pii/S1556407X14001246#preview-section-cited-by
- Tobaldini E, Costantino G, Solbiati M, Cogliati C, Kara T, Nobili L, Montano N. Sleep, sleep deprivation, autonomic nervous system and cardiovascular diseases. Neurosci Biobehav Rev. 2017 Mar;74(Pt B):321-329. doi: 10.1016/j.neubiorev.2016.07.004. Epub 2016 Jul 7. PMID: 27397854.
- Hansmann, R., Hug, S.-M., & Seeland, K. (2007, October 18). Restoration and stress relief through physical activities in forests and Parks. Urban Forestry & Urban Greening. https://www.sciencedirect.com/science/article/abs/pii/S1618866707000623
- Kellert, S. R., & Wilson, E. O. (1993). The biophilia hypothesis. Google Books. https://books.google.ca/books?hl=en&lr=&id=GAO8BwAAQBAJ&oi=fnd&pg=PP6&ots=pmvcPCBUs-&sig=7gNRk_RtavkfhfxogMKNBe1_COE&redir_esc=y#v=onepage&q&f=false
- Kaplan, R., & Kaplan, S. (1989). The experience of nature. Google Books. https://books.google.ca/books?hl=en&lr=&id=7l80AAAAIAAJ&oi=fnd&pg=PR7&ots=TqP_VHm5Yk&sig=EMk6-LKluPnjaCFaM8-aMtaKG80&redir_esc=y#v=onepage&q&f=false
- Ulrich RS. View through a window may influence recovery from surgery. Science. 1984 Apr 27;224(4647):420-1. doi: 10.1126/science.6143402. PMID: 6143402.
- Ulrich, R. S., Simons, R. F., Losito, B. D., Fiorito, E., Miles, M. A., & Michael Zelson, M. (1991). Stress recovery during exposure to natural and urban environments. Journal of Environmental Psychology. https://doi.org/10.1016/S0272-4944(05)80184-7
- Kondo MC, Jacoby SF, South EC. Does spending time outdoors reduce stress? A review of real-time stress response to outdoor environments. Health Place. 2018 May;51:136-150. doi: 10.1016/j.healthplace.2018.03.001. Epub 2018 Mar 29. PMID: 29604546.
- Jimenez MP, DeVille NV, Elliott EG, Schiff JE, Wilt GE, Hart JE, James P. Associations between Nature Exposure and Health: A Review of the Evidence. Int J Environ Res Public Health. 2021 Apr 30;18(9):4790. doi: 10.3390/ijerph18094790. PMID: 33946197; PMCID: PMC8125471.
- Holt EW, Lombard QK, Best N, Smiley-Smith S, Quinn JE. Active and Passive Use of Green Space, Health, and Well-Being amongst University Students. Int J Environ Res Public Health. 2019 Feb 1;16(3):424. doi: 10.3390/ijerph16030424. PMID: 30717193; PMCID: PMC6388138.
- Wang P, Meng YY, Lam V, Ponce N. Green space and serious psychological distress among adults and teens: A population-based study in California. Health Place. 2019 Mar;56:184-190. doi: 10.1016/j.healthplace.2019.02.002. Epub 2019 Feb 21. PMID: 30797185.
- McCormick R. Does Access to Green Space Impact the Mental Well-being of Children: A Systematic Review. J Pediatr Nurs. 2017 Nov-Dec;37:3-7. doi: 10.1016/j.pedn.2017.08.027. Epub 2017 Sep 4. PMID: 28882650.
- Radin RM, Mason AE, Laudenslager ML, Epel ES. Maternal caregivers have confluence of altered cortisol, high reward-driven eating, and worse metabolic health. PLoS One. 2019 May 10;14(5):e0216541. doi: 10.1371/journal.pone.0216541. Erratum in: PLoS One. 2019 Aug 14;14(8):e0221354. PMID: 31075126; PMCID: PMC6510426.
- Yau YH, Potenza MN. Stress and eating behaviors. Minerva Endocrinol. 2013 Sep;38(3):255-67. PMID: 24126546; PMCID: PMC4214609.
- Esch T, Stefano GB. Endogenous reward mechanisms and their importance in stress reduction, exercise and the brain. Arch Med Sci. 2010 Jun 30;6(3):447-55. doi: 10.5114/aoms.2010.14269. PMID: 22371784; PMCID: PMC3282525.
- Esch T, Stefano GB. The neurobiology of stress management. Neuro Endocrinol Lett. 2010;31(1):19-39. PMID: 20150886.
- Balban MY, Neri E, Kogon MM, Weed L, Nouriani B, Jo B, Holl G, Zeitzer JM, Spiegel D, Huberman AD. Brief structured respiration practices enhance mood and reduce physiological arousal. Cell Rep Med. 2023 Jan 17;4(1):100895. doi: 10.1016/j.xcrm.2022.100895. Epub 2023 Jan 10. PMID: 36630953; PMCID: PMC9873947.
- Estevao C. The role of yoga in inflammatory markers. Brain Behav Immun Health. 2022 Feb 1;20:100421. doi: 10.1016/j.bbih.2022.100421. PMID: 35199049; PMCID: PMC8842003.
- Fincham GW, Strauss C, Montero-Marin J, Cavanagh K. Effect of breathwork on stress and mental health: A meta-analysis of randomised-controlled trials. Sci Rep. 2023 Jan 9;13(1):432. doi: 10.1038/s41598-022-27247-y. PMID: 36624160; PMCID: PMC9828383.
Daniel DeBrocke is the director of education curriculum at Kabuki Strength. He's a competitive powerlifter and strength coach with over ten years of experience in the field. He has coached athletes ranging from novice lifters to world record holders, national champion BMX racers, and professional soccer and MLB players.
Daniel is a published author and writes for several renowned publications such as elitefts, Kabuki Strength, T-Nation, Bar Bend, Breaking Muscle, and Evil Genius Sport Performance. He has presented at international conferences alongside industry experts. Daniel is also the creator of the Stacked Strength Podcast.










1 Comment